Me and My Operation: Kerry Taylor

Remote control that can switch off that agonising back pain
The Patient
While hula hooping with my daughter Ciara - then five - one summer, I suddenly felt a strange sensation in my back, as if something inside was being crumpled.
It didn’t hurt, but was very odd. However, the next morning, I felt a searing pain down my right leg and buttock.
I called my mother, who drove me to A&E, where they diagnosed sciatica. They explained this happens when the gel-like inner contents of a disc in the spine starts bulging out and pressing down on the sciatic nerve. They thought it would heal naturally in sex weeks, and sent me home with painkillers.
But the painkillers didn’t help. From that day on, in August 2010, I was in constant agony - just turning over in bed would send the nerve into spasm, causing painful cramps in my leg. I couldn’t lift my one-year-old daughter, Edel, so my partner Peter had to give up work to look after us.
I was working in a supermarket at the time, but lost my job because putting any pressure on my right foot set the spasms off, so I couldn’t walk without crutches.
For eight months I was basically bed bound and in great pain. And there were many times when I had to be taken to hospital by ambulance after collapsing from a massive spasm in my back.
I saw my GP several times, and was prescribed various painkillers and muscle relaxants - I was taking 27 different pills a day, but they mainly just made me woozy.
So, in April 2011, I had surgery to remove the bulging disc. But I was still in as much pain afterwards, as the sciatic nerve was badly damaged.
My GP referred me to the pain clinic at Whipps Cross Hospital in London, where, in early 2012, I was given nerve block injections into my spine, and jabs to reduce inflammation.
These helped for a while, so Peter went back to work and I was able to start volunteering in Edel’s pre-school. But, last May, the pain began to get worse again, the awful spasms returned, and I had to give that up. I was in tears when my pain consultant said there was no more he could do. However, he mentioned spinal cord stimulation might help, although it was not available at his clinic.
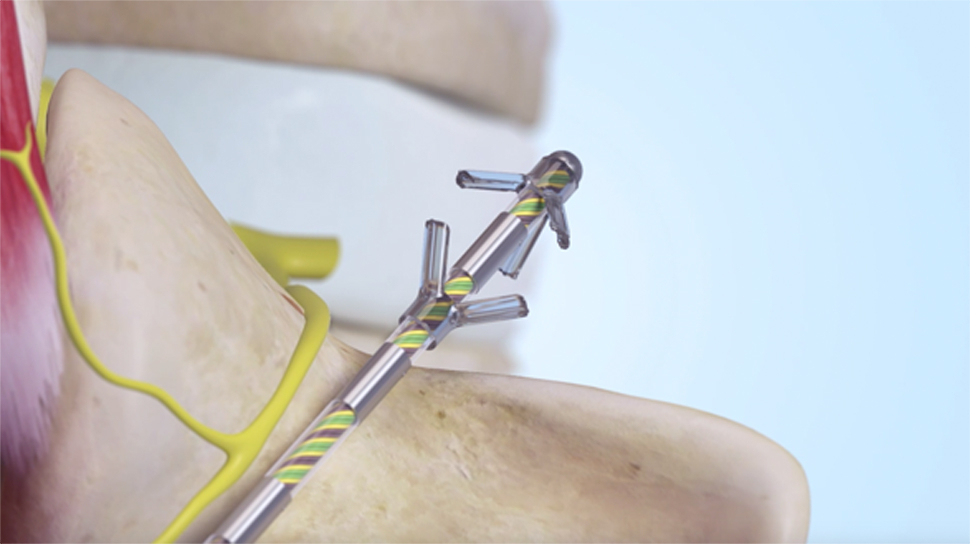
This would involve having electrodes placed in my spine, close to the damaged nerve, which would send impulse that would block the pain signals.
In June, I saw Vivek Mehta, a consultant in pain medicine at Barts Hospital in London. He explained he was using a new type of stimulator - older versions send a single impulse to block pain signals. This new type sent two different types - one would be fired in a regular pattern, the other faster, in intermittent bursts.
This was meant to work better than just one impulse. I felt I had nothing to lose.
In January, I had the two-hour operation to implant the electrodes, under sedation - I needed to be awake so Dr Mehta could stimulate different areas of my spinal cord and I could tell him when he’d hit the rights spot and the pain had gone.
For a week, I had wires sticking out of my back, connected to a temporary battery I carried in a handbag. This was slightly strange, but the main thing was I had no pain at all and I couldn’t feel the implant either. For the first time in years, I slept soundly.
A week later I had a second, 20-minute operation, sedated and with local anaesthetic, to implant a permanent battery above my buttock. Twice a week I have to wear a special belt that charges the battery through my skin - this takes under two hours.
I use a remote control to switch the device on twice a day, for five hours at work and while I sleep.
Its basically trained my nerves so that they don’t transmit pain even when the implant is off, and I’m finding that the longer I have it, I don’t even need to use it quite this much. Now I’ve managed to qualify as a pre-school teacher and am back at work.
I’m even planning to marry Peter this year now we don’t need to worry about pain. It’s just amazing.
The Consultant
Vivek Mehta is a consultant in pain medicine at St Bartholomew’s Hospital in London.
MILLIONS of Britons have chronic back or leg pain, often caused by damage to nerves in the spinal cord brought on by a bulging disc - known as a slipped disc - that then presses on a nerve.
Even after surgery to remove the bulging disc, 30 to 40 per cent of people have pain because the nerve has been damaged, or as a result of scarring from the surgery.
Painkillers can help, and we can also try injections into the spine to reduce inflammation and pain.
But when all else fails, we can offer spinal cord stimulation - where electrodes are implanted close to nerves in the spine. These fire signals that should override pain signals and block the pain.
This is effective in many patients, but doesn’t work for everyone. And the continuous signals being fired by the implant can cause some people to feel a tingling sensation down the leg, which can be very uncomfortable.
But a new system, known as Prodigy with Burst technology, can overcome this problem. Licensed for use in Europe last year, it uses two different signals to block the pain, rather than a single one as used in devices up until now.
These both block the existing pain and leave the patient free of any uncomfortable tingling.
As well as firing out regular, even signals, at 30 to 40 times a second, it also produces intermittent bursts of rapid-fire stimulation.
These short bursts are thought to mimic the firing of the nerve cells in the body that transmit pain, and are therefore more effective at blocking it. The pain is up to 44 per cent better controlled that with the older-style stimulators.
The operation takes 90 minutes to two hours. The patient is sedated, so that we can be sure we simulate the right part of the spinal cord during the procedure to take their pain away. First, we use a large needle to inject two electrodes next to the spinal cord. Then we make a 1-2cm incision in the lower back and stitch the electrodes to the muscle in the back. We then tunnel wires under the skin just above the buttock and connect the electrodes to a temporary battery. We close the incision with stitches, covering it with a dressing.
ONCE we are sure it works, the patient has a second 20-minute operation a week or so later. I make a 5cm incision above the buttock and tuck the battery - which is 5cm by 5cm - under the skin, closing the incision with stitches. I feed the wires into the holes in the battery, and tighten it with a screwdriver.
The battery should last about ten years before it needs replacing.
A study published in the journal World Neurosurgery last year found Prodigy gave better control of pain than conventional spinal cord stimulation, without causing tingling or discomfort.
Any Drawbacks?
THE operation carries risks including bleeding and infection, and a very slight risk of a leak of cerebrospinal fluid, the clear fluid around brain spine, which would cause a headache for a couple of days but is not dangerous.
’Spinal cord stimulation carries a risk that the leads in the back could break or move, which means a second operation to reposition them,’ adds Ganesan Baranidharan, consultant in pain medicine at Leeds Teaching Hospitals NHS Trust.
‘There is also a very small risk of paralysis. But unlike previous spinal cord stimulation, Prodigy effectively speaks the same language as the nervous system. It is therefore more effective in overcoming pain and means that patients should not have the tingling or discomfort that older techniques can cause.’
- The operation costs around £18,000 to 20,000 privately or to the NHS.
Source: Daily Mail, Tuesday March 31 2015
View the full article here: Kerry Taylor