Battery-Powered Back Pain Relief
With our increasingly sedentary lifestyle, lower back pain is becoming a common complaint among the over-50s. This debilitating condition already affects an estimated 40 per cent of the UK population.
While many sufferers get better thanks to physiotherapy and exercise, those with degenerative disc disease – where the gel-filled discs between the bones in their spine wear out – continue to be in agonising pain. Taking painkillers and having steroid injections offer them little respite as the discs rub and grind against each other.
Now, however, an implantable stimulation system that the patient controls with a hand-held remote is helping to provide this group of patients with significant pain relief when it is used for 30 minutes twice a day for 90 days. When they use the device, patients have to lie on their fronts and it can take time for them to become accustomed to the electrical pulses it emits.
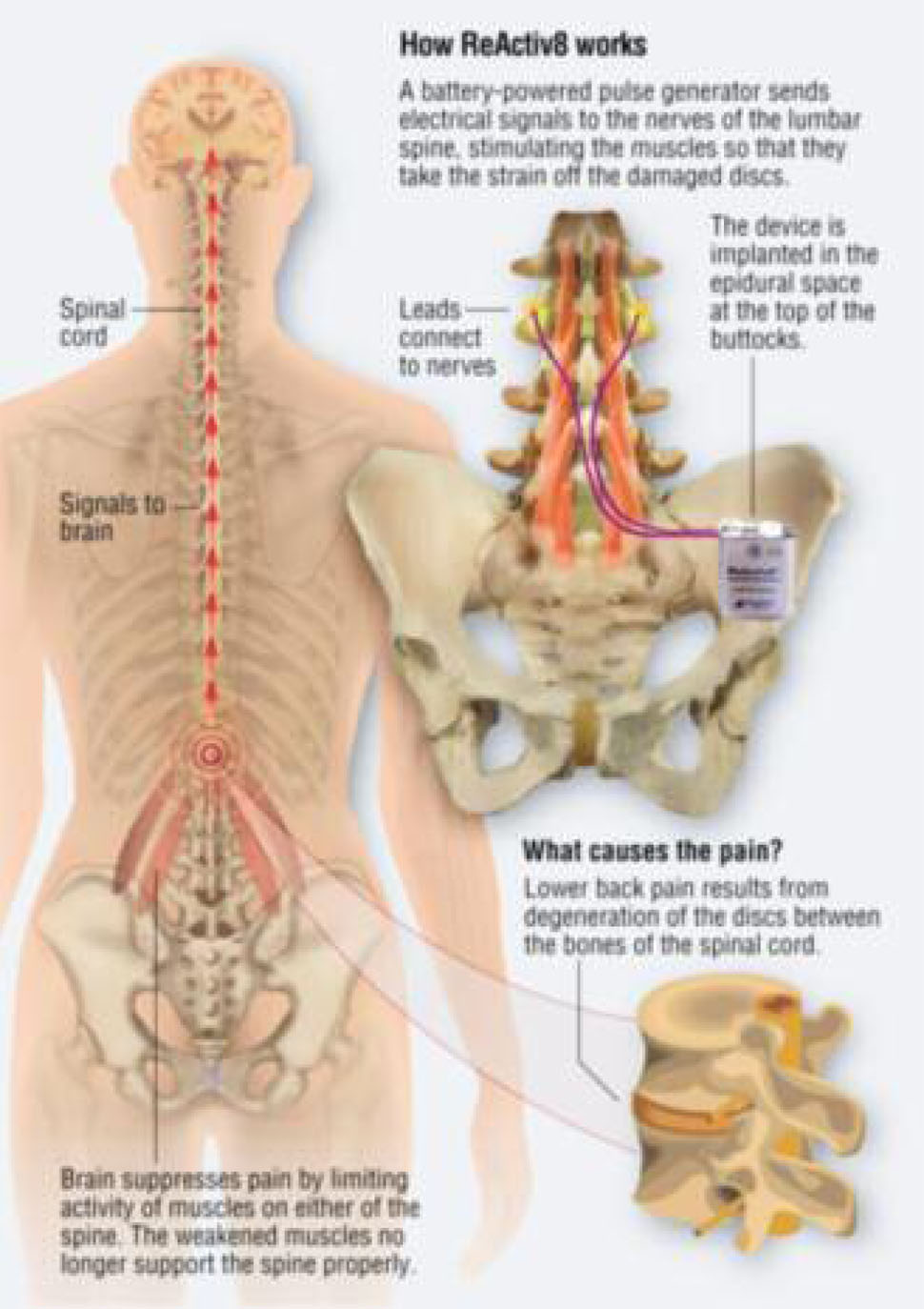
Illustration by Michael Roscoe
Dr Vivek Mehta, a consultant in pain medicine at Bart’s Hospital in London, who is participating in trials of the device, explains: “We estimate that two in every five cases of lower back pain are the result of degenerative disc disease where the gel-filled discs between the bones in the spine wear out, causing inflammation and pain. When this occurs, the brain tries to suppress painful movements by limiting the activity of the muscles on either side of the spine but this only makes matters worse. These muscles get weaker and as a result can no longer support the spine properly. Because it is no longer being properly supported, more pressure is put on the damaged discs so the patient ends up in even more pain.”
He adds: “This new treatment can help relieve this type of pain and break the cycle of chronic pain the patient is in. It does this by getting weakened muscles in the lower back to start working again and building up their strength. When they get stronger, the muscles take the strain off the damaged spine, which reduces the pain.”
Called ReActiv8, the device has been developed by Mainstay Medical, a Dublin-based company, and is already approved for use in Europe. Currently it is available on the NHS only at centres taking part in the trials. Privately it costs around £18,000.
Initial trial results, presented in June, showed that the device, which has a battery life of five years, had brought pain relief to 63 per cent of patients after 90 days and had improved their quality of life by 80 per cent.
Its use enabled many to substantially reduce the amount of painkilling medication they were taking and some were able to come off medication altogether.
Dr Mehta describes this response as ‘phenomenal’ and says the device is a major step forward in the treatment of lower back pain. He is optimistic that if trial results continue to demonstrate that ReActiv8 helps to relieve chronic lower back pain, it will soon become more generally available.
Dr Mehta says: “Before we implant the device, we have to ensure the patient’s lower back pain is not due to other causes such as nerve compression, a protruding disc or a fracture.” To establish the underlying cause, MRI scans and X-rays are done. “In most cases,” Dr Mehta says, “the problem is due to degenerative disc disease, but before finally going ahead we have to be certain that the patient is sufficiently motivated to use the device.
“For this treatment to be successful the patient needs to switch the device on and use it for 30 minutes every morning and evening. Then the stimulation it provides will start to get the muscles in their lower back working again, and it is this that helps patients to get better.”
Dr Mehta points out: “We find most people affected by lower back pain are middle-aged. By the time they reach 50, sitting at a computer all day and not being that active has taken its toll. Initially patients with this kind of lower back pain are given physiotherapy and painkillers such as Tramadol and Gabapentin. Steroid injections which can help to reduce inflammation are also tried.” When patients fail to respond to these treatments, they are referred to a specialist pain clinic and could be considered for the implantable device.
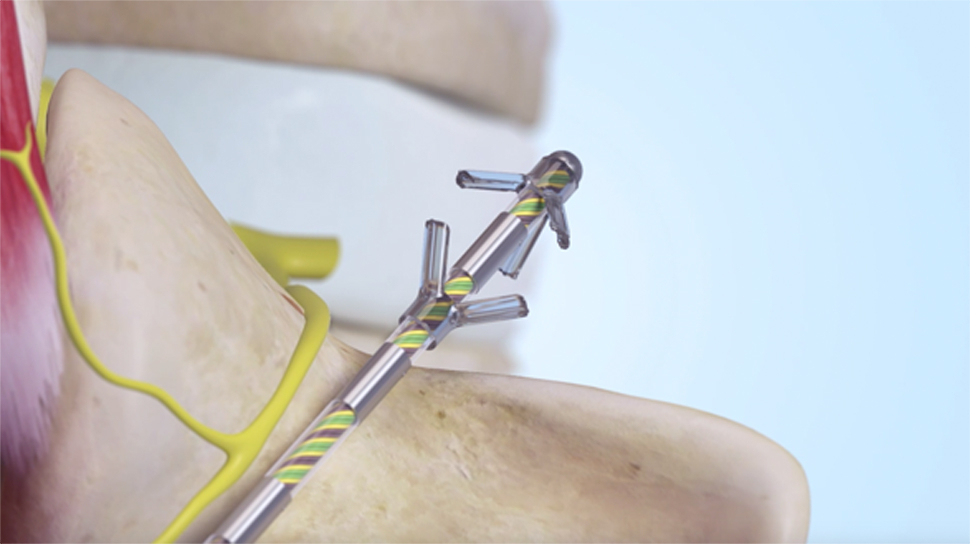
The procedure, which takes one and a half to two hours, is performed under a general anaesthetic. Using X-ray guidance, electrodes are fitted inside the muscles on either side of the spine and connected to the device itself, which is implanted in the lower lumbar region.
The patient is then given a hand-held remote to switch the device on and off and to control the frequency. The device then stimulates the nerves responsible for activating the muscles in the lower back. Dr Mehta describes the battery-powered device as ‘internal physiotherapy’.
Sharon Palmer: Depressed and frustrated by lower back pain
Sometimes, when the pain in her lower back was so bad, the only way Sharon Palmer, from Hornchurch in Essex, could get round was to crawl.
For Sharon, 55, a former care home manager and mum of four, everyday activities such as standing to brush her teeth and prepare dinner made her pain worse, and just walking small distances began to be a huge problem.
Her pain started 20 years ago. Sharon says there was no confirmed reason for it and her GP told her it was “just one of those things”.
“I went back to see him several times and was prescribed different painkillers but none of them were able to control the pain. Twelve years after my pain had started, I had no choice but to give up work.
“This made me feel useless and there were times when I thought about ending it all. It was only the thought of my children, grandchildren and partner that kept me going.
“My partner had to help me get out of bed in the morning, and to sit and stand up and to go to the toilet because I could not lower myself on or off it. In fact, every part of my life required assistance from others.
“I got depressed and frustrated because it was so hard to cope. Even socialising was an issue because I had to sit down wherever I went and, if no chairs were available, I had to come home and would have to take a taxi. I was unable to use public transport because I couldn’t get to the bus stop or railway station in the first place.”
Four years ago Sharon insisted her GP referred her to the specialist pain clinic at St Bartholomew’s Hospital in London. She says: “I had to make the request four times before he took me seriously and he only agreed because I said I would report him for lack of duty of care if he did not.”
At Bart’s, an MRI scan and X-ray showed that Sharon was suffering from lumbar spondylosis, which meant the discs in her spine were crumbling away and pinching her nerves. At the same time, her brain was issuing messages to stop her back muscles from being activated to prevent movement and thereby curb her pain.
Instead, this made her pain worse because it meant these were growing weaker and were therefore unable to adequately support her spine. Despite having steroid injections, her pain would return two to three weeks later.
By now Sharon was willing to try anything to get rid of her pain, and was considering surgery to fuse the bones in her back, when she was asked if she would be willing to participate in a trial of a new implanted device.
She says: “I was reluctant at first but being in so much pain the decision to go for it was easy. I was desperate.”
In March 2015, the device that delivers electrical pulses to stimulate and strengthen the muscles on either side of Sharon’s spine was implanted.
She has a remote to control the strength of the pulses and uses the device for 30 minutes twice a day. Sharon adds: “After the op, I was unsure if I’d made the right decision because it took me about three months to get used to the machine in my back. I have to lie on my front while the remote sends out signals and it is a funny sensation. The pulses go down your spine for 20 seconds then your muscles tense and the pulses stop for ten seconds before they start up again.
“But this device has enabled me to get my life back and I’m feeling happy again. I’m able to play with my grandchildren and have a new job working as a phlebotomist.
“I still take morphine-based painkillers but thanks to the device my back pain is now bearable. On an average day, it has gone down from 100 per cent to 15 per cent, which I can live with.
Source: CHOICE FEBRUARY 2018
View the full article here: Battery-Powered Back Pain Relief